EHR Pricing Guide 2025: Complete Cost Breakdown
Epic implementation costs vary dramatically based on organization size and complexity. Small health systems typically invest $2-5 million for basic implementations, while large academic medical centers may spend $50-100 million or more for comprehensive deployments.
Electronic Health Records (EHR) have revolutionized healthcare delivery, transforming how medical professionals manage patient information, streamline workflows, and ensure regulatory compliance. However, implementing electronic health record EHR software represents one of the most significant technology investments healthcare organizations make. Understanding the comprehensive EHR pricing structure is crucial for making informed decisions that align with both clinical needs and financial constraints.
1. What is EHR and Why Pricing Matters
Electronic Health Records are digital versions of patients’ paper charts, containing comprehensive medical histories, diagnoses, medications, treatment plans, immunization dates, allergies, radiology images, and laboratory test results. Electronic medical records software enables healthcare providers to access patient information instantly, share data securely across departments, and maintain accurate records that support quality care delivery.
EHR pricing matters significantly because electronic health record software implementation costs extend far beyond initial software purchases. The average cost of an EHR system is $1,200 per year per user, but this figure represents only the beginning of total ownership costs. Healthcare organizations must consider direct expenses, hidden fees, ongoing maintenance, staff training, and potential system upgrades when budgeting for electronic medical health records software implementation.
The financial impact of electronic health record EHR software selection affects healthcare organizations for years, influencing operational efficiency, patient satisfaction, and overall profitability. Poor planning or underestimating EHR pricing can lead to budget overruns, implementation delays, and suboptimal system performance that ultimately compromises patient care quality.
2. EHR Cost Breakdown
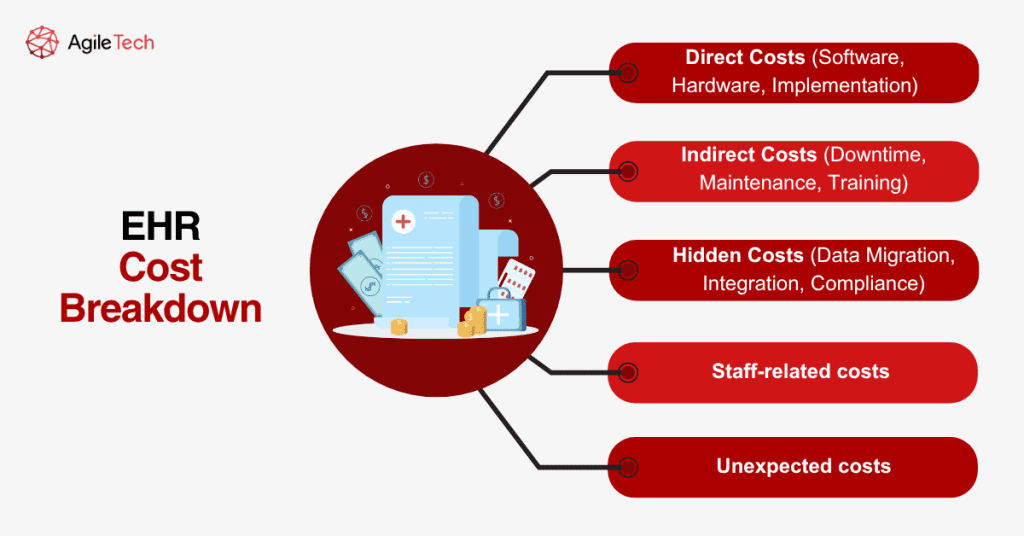
2.1. Direct Costs (Software, Hardware, Implementation)
Direct costs represent the most visible expenses in electronic medical records software implementation. Software licensing constitutes the primary expense, varying dramatically based on system complexity, user count, and deployment model. Cloud-based electronic health record software typically charges monthly or annual subscription fees, while on-premise systems require substantial upfront investments.
Hardware requirements include servers, workstations, mobile devices, networking equipment, and backup systems. Cloud-based electronic health record EHR software reduces hardware needs significantly, as vendors handle server infrastructure, but organizations still need endpoints, networking gear, and backup solutions.
Implementation costs encompass system configuration, data migration, workflow customization, and integration with existing systems. Professional services from electronic medical health records software vendors or third-party consultants typically charge hourly rates ranging from $150 to $300, with total implementation requiring hundreds or thousands of professional hours, depending on organization size and complexity.
2.2. Indirect Costs (Downtime, Maintenance, Training)
Indirect costs often surprise healthcare organizations because they’re less obvious during initial EHR pricing evaluation phases. System downtime during implementation and ongoing maintenance creates productivity losses, delayed appointments, and potential revenue reduction. Organizations typically experience 20-30% productivity decreases during the first few months after electronic medical records software implementation.
Maintenance costs include software updates, security patches, system monitoring, and technical support. Healthcare organizations allocate 15-20% of their electronic health record software implementation budget to these services, ensuring successful adoption and operation throughout the system lifecycle.
Training represents another significant indirect cost, requiring comprehensive education for all users from physicians to administrative staff. Initial training typically requires 20-40 hours per user, with ongoing education needed for electronic health record EHR software updates, new features, and staff turnover replacement.
2.3. Hidden Costs (Data Migration, Integration, Compliance)
Hidden costs emerge throughout electronic medical health records software implementation and operation, often catching organizations unprepared. Data migration from legacy systems requires extensive planning, testing, and validation to ensure accuracy and completeness. Complex data structures, inconsistent formats, and regulatory requirements make migration challenging and expensive.
Integration costs arise when connecting electronic health record software with existing healthcare applications, medical devices, laboratory systems, and third-party services. Each integration point requires custom development, testing, and ongoing maintenance to ensure seamless data flow.
Compliance costs include regulatory requirements for HIPAA security, meaningful use certification, and quality reporting programs. Organizations must invest in security infrastructure, audit capabilities, and compliance monitoring to meet regulatory standards and avoid penalties.
2.4. Staff-related Costs
Staff-related costs encompass training, productivity losses, and potential staffing changes required for successful electronic health record EHR software implementation. Clinical staff need extensive training on new workflows, documentation requirements, and system navigation. Administrative staff require training on scheduling, billing, and reporting functions.
Productivity losses during transition periods can last several months as staff adapt to new electronic medical records software and workflows. Some organizations hire temporary staff or consultants to maintain operations during implementation phases, adding to overall EHR pricing.
Long-term staffing changes may include hiring IT support personnel, clinical informaticists, or system administrators to manage ongoing electronic health record software operations and optimization.
2.5. Unexpected Costs
Unexpected costs frequently arise during electronic medical health records software implementation, often related to scope changes, technical challenges, or regulatory requirements. System customization beyond initial plans can significantly increase EHR pricing, especially for complex clinical workflows or specialty-specific requirements.
Hardware failures, network upgrades, or security breaches may require unplanned investments in infrastructure or remediation services. Regulatory changes or vendor policy updates can force system modifications or compliance upgrades at additional expense.
Performance issues may necessitate hardware upgrades, network improvements, or additional professional services to achieve acceptable electronic health record EHR software response times and user satisfaction.
Read more: Telemedicine Software Development: Types, Benefits, and How to Build It Right?
3. EHR Pricing Models
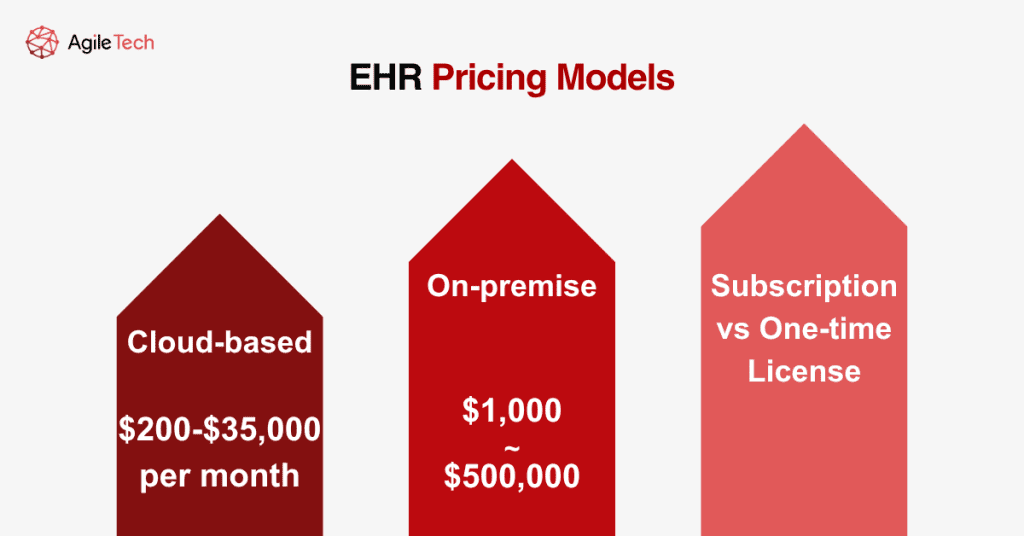
3.1. Cloud-based ($200-$35,000/month)
Cloud-based electronic medical records software offers flexible pricing models with monthly or annual subscription fees. The cost of Epic can range anywhere between $200 to $35,000 per month, depending on organization size, features, and customization requirements. Smaller practices typically pay $200-$800 per provider monthly, while large health systems may exceed $10,000 monthly for comprehensive implementations.
Cloud EHR pricing advantages include predictable monthly expenses, automatic updates, and reduced IT infrastructure requirements. Vendors handle server maintenance, security updates, and system backups, reducing internal IT burden and costs.
Disadvantages include ongoing subscription costs, data control concerns, and potential vendor lock-in situations. Organizations must carefully evaluate long-term electronic health record software costs versus benefits when considering cloud-based solutions.
3.2. On-premise ($1,000-$500,000)
On-premise electronic health record EHR software requires substantial upfront investments ranging from $1,000 for basic systems to over $500,000 for enterprise implementations. Mayo Clinic announced plans to move to an Epic EHR system, costing more than $1.5 billion over five years, demonstrating the scale of large-scale implementations.
On-premise advantages include complete data control, customization flexibility, and no ongoing subscription fees after initial implementation. Organizations maintain full control over electronic medical health records software configuration, security policies, and upgrade timing.
Disadvantages include high upfront costs, ongoing maintenance responsibilities, and internal IT expertise requirements. Organizations must budget for hardware refreshes, software updates, and security management throughout the electronic health record software lifecycle.
3.3. Subscription vs One-time License
Subscription models spread EHR pricing over time with predictable monthly or annual payments. This approach reduces initial capital requirements and includes ongoing support, updates, and maintenance services. Subscription pricing typically ranges from $25 to $1,500 per provider monthly, depending on the electronic medical records software complexity and features.
One-time license models require substantial upfront payments but eliminate ongoing subscription fees. Organizations own the electronic health record EHR software permanently but must separately purchase maintenance contracts, updates, and support services. License costs range from $1,000 to $15,000 per provider, with additional fees for implementation and customization.
The choice between subscription and license models depends on organization size, financial preferences, and long-term strategic plans. Smaller practices often prefer subscriptions for cash flow management, while larger organizations may favor licensing for long-term electronic health record software cost control.
4. Popular EHR Systems Pricing
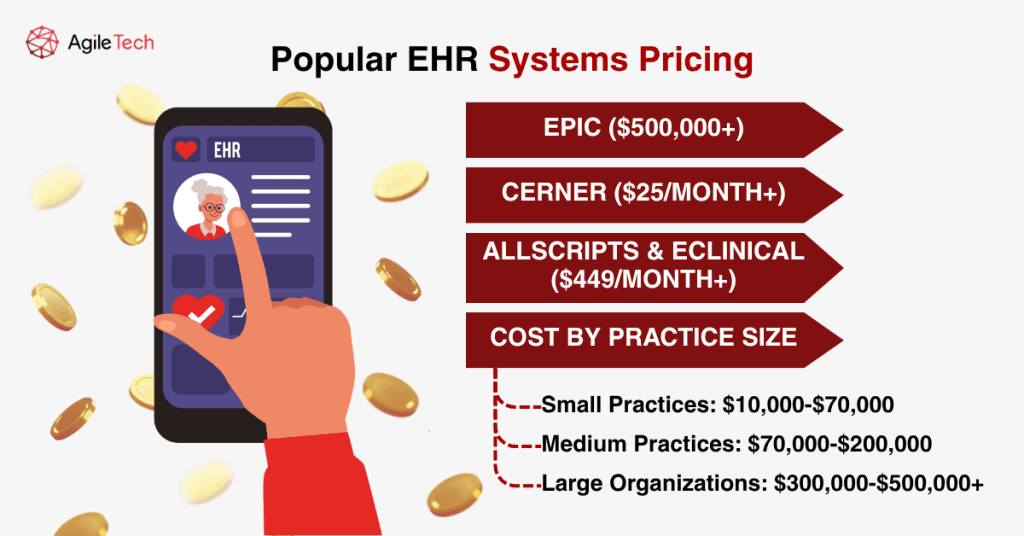
4.1. Epic ($500,000+)
Epic represents the premium tier of electronic medical health records software, serving large health systems and academic medical centers. Epic typically charges $5,000–$7,000 per user for physician licenses, with total implementation costs frequently exceeding $500,000 for mid-sized organizations and reaching millions for large health systems.
Epic’s comprehensive functionality includes clinical documentation, revenue cycle management, patient engagement tools, and population health analytics. The electronic health record EHR software integration capabilities and interoperability features make it attractive for complex healthcare organizations requiring enterprise-level functionality.
Implementation timelines typically range from 12-24 months, with extensive customization and training requirements. Organizations must budget for significant change management efforts and productivity losses during electronic health record software transition periods.
4.2. Cerner ($25/month+)
Cerner, now part of Oracle Health, offers flexible EHR pricing options for various organization sizes. Cerner offers an annual subscription plan for its basic cloud-based solution for $25 a month for individual practitioners, while enterprise implementations require custom quotes based on specific requirements.
Cerner’s scalability makes it suitable for practices ranging from small clinics to large health systems. The electronic medical records software includes clinical documentation, population health tools, and revenue cycle management capabilities.
Cloud-based Cerner implementations typically cost $25-$200 per provider monthly, while on-premise deployments vary widely based on customization and integration requirements for the electronic health record EHR software.
Read more: Healthcare ERP Solutions: Optimizing Medical Processes & Patient Care
4.3. Allscripts & eClinical ($449/month+)
Allscripts (now Veradigm) offers multiple EHR pricing tiers to accommodate different practice sizes and needs. It offers two pricing plans: the Practice Fusion EHR plan that starts from $149/month and the Veradigm ePrescribe plan, which starts from $59/month/prescriber. The AI-powered electronic health record software costs $449 per month, and the EHR with practice management costs $599 per month.
Allscripts: Subscription plans often start around $500–$1,500 per provider per month, making it a cost-effective option for smaller practices seeking to avoid Epic’s higher costs while maintaining comprehensive electronic medical health records software functionality.
eClinicalWorks provides another mid-market option with competitive EHR pricing and specialty-specific features. The electronic health record EHR software includes practice management, patient engagement tools, and revenue cycle management capabilities.
| EHR System | Starting Price | Enterprise Price | License Cost | Target Market | Key Features |
| Epic | $500,000+ | $50M+ | $5,000-$7,000/user | Large health systems | Enterprise integration, comprehensive |
| Cerner | $25/month | Custom quote | $25-$200/provider/month | All sizes | Scalable, Oracle-backed |
| Allscripts | $149/month | $1,500/provider/month | $500-$1,500/provider | Small-medium practices | Cost-effective, AI-powered |
| eClinicalWorks | $449/month | Custom quote | Varies | Mid-market | Specialty-focused, competitive pricing |
4.4. Cost by Practice Size
Small Practices: $10,000-$70,000
Small practices (1-10 providers) typically invest $10,000-$70,000 for complete electronic medical records software implementation. This range includes software licensing, basic customization, training, and initial support services. Cloud-based solutions often represent the most cost-effective option for small practices, providing enterprise-level functionality without substantial upfront investments in electronic health record software.
Medium Practices: $70,000-$200,000
Medium practices (11-50 providers) generally invest $70,000-$200,000 for comprehensive electronic health record EHR software implementation. These organizations require more extensive customization, integration capabilities, and support services than smaller practices. Multiple specialty workflows, advanced reporting requirements, and integration with ancillary systems drive higher EHR pricing.
Large Organizations: $300,000-$500,000+
Large organizations (50+ providers) typically invest $300,000-$500,000 or more for enterprise electronic medical health records software implementation. These implementations require extensive customization, multiple system integrations, comprehensive training programs, and ongoing support services. Complex workflows, regulatory requirements, and interoperability needs significantly increase implementation costs and timelines.
| Practice Size | Provider Count | Investment Range | Key Requirements | Implementation Time | Complexity Level |
| Small Practices | 1-10 providers | $10,000-$70,000 | Basic EHR, cloud-based | 3-6 months | Low |
| Medium Practices | 11-50 providers | $70,000-$200,000 | Customization, integration | 6-12 months | Medium |
| Large Organizations | 50+ providers | $300,000-$500,000+ | Enterprise features, multiple integrations | 12-24 months | High |
5. Hidden Costs of Implementing EHR
Hidden costs represent one of the most challenging aspects of EHR pricing budgeting because they’re difficult to anticipate and quantify during initial planning phases. Data migration costs often exceed initial estimates due to data quality issues, format incompatibilities, and validation requirements. Organizations frequently discover data inconsistencies or missing information that require manual correction or additional development work for electronic health record software.
Interface development costs arise when integrating electronic medical records software with existing applications, medical devices, or third-party services. Each integration point requires custom development, testing, and ongoing maintenance that wasn’t included in initial pricing estimates.
Workflow redesign costs emerge as organizations adapt clinical and administrative processes to work optimally with new electronic health record EHR software. This may require additional consulting services, extended training programs, or temporary staffing to maintain operations during transition periods.
Compliance costs include security infrastructure, audit capabilities, and regulatory reporting tools needed to meet HIPAA, meaningful use, and quality reporting requirements. Organizations must invest in additional security measures, monitoring tools, and compliance documentation that weren’t included in basic electronic medical health records software pricing.
6. Cost of Implementing Popular EHR Solutions
6.1. Epic
Epic implementation costs vary dramatically based on organization size and complexity. Small health systems typically invest $2-5 million for basic implementations, while large academic medical centers may spend $50-100 million or more for comprehensive deployments. NYC Health + Hospitals began rolling out its $1 billion Epic EHR, demonstrating the scale of enterprise implementations.
Implementation timelines typically range from 18-36 months, with extensive planning, customization, and training phases. Organizations must budget for significant change management efforts, temporary staffing, and productivity losses during go-live periods.
Ongoing costs include annual maintenance fees (typically 15-20% of license costs), hosting services, and support contracts. Organizations should budget for system upgrades, additional modules, and expanded functionality over time.
6.2. Cerner
Cerner implementation costs depend on the deployment model and organization size. Cloud-based implementations for small practices may cost $50,000-$200,000, while large health system deployments can exceed $10 million. Implementation timelines typically range from 6-18 months, depending on complexity and customization requirements.
Oracle’s acquisition of Cerner has introduced uncertainty regarding future pricing and support policies. Organizations should carefully evaluate long-term vendor stability and migration options when considering Cerner implementations.
6.3. Allscripts
Allscripts implementation costs typically range from $25,000-$500,000 depending on practice size and feature requirements. Small practices can implement basic EHR functionality for $25,000-$75,000, while larger organizations require $200,000-$500,000 for comprehensive implementations.
Implementation timelines generally range from 3-12 months, with simpler deployments completing faster than complex, multi-site implementations. Allscripts’ focus on ambulatory care makes it particularly suitable for physician practices and outpatient clinics.
6.4. eClinical
eClinicalWorks implementation costs typically range from $30,000-$300,000 for most practice sizes. The vendor’s focus on providing comprehensive solutions at competitive prices makes it attractive for cost-conscious organizations seeking full-featured EHR systems.
Implementation timelines typically range from 2-8 months, with the vendor providing extensive support services to ensure successful deployments. eClinicalWorks includes practice management, patient engagement, and revenue cycle management tools in most packages.
| EHR System | Implementation Cost Range | Timeline | Best For | Key Advantages |
| Epic | $2M-$100M+ | 18-36 months | Large health systems | Comprehensive, enterprise-grade |
| Cerner | $50,000-$10M+ | 6-18 months | All sizes | Scalable, Oracle support |
| Allscripts | $25,000-$500,000 | 3-12 months | Small-medium practices | Cost-effective, ambulatory focus |
| eClinicalWorks | $30,000-$300,000 | 2-8 months | Cost-conscious organizations | Comprehensive, competitive pricing |
Read more: How to Create Pharmacy Management System: Full Process Explained
7. Main Factors That Influence EHR Implementation Cost
Several key factors significantly influence EHR implementation costs. Organization size represents the primary cost driver, as larger practices require more user licenses, extensive customization, and complex integration requirements. The worldwide market for Clinical EHR Systems will expand from a valuation of $19.66 billion in 2023 to reach approximately $26.50 billion by 2028, indicating continued growth and investment in EHR technology.
Customization requirements substantially impact costs, as specialty-specific workflows, custom forms, and unique reporting needs require additional development work. Organizations with standard workflows typically achieve lower implementation costs than those requiring extensive customization.
Integration complexity affects costs significantly, as connections to laboratory systems, imaging equipment, pharmacy systems, and third-party applications require custom development and ongoing maintenance. Organizations with multiple existing systems typically face higher integration costs.
Data migration complexity influences costs based on legacy system types, data quality, and migration requirements. Organizations with clean, well-structured data typically achieve lower migration costs than those with inconsistent or incomplete historical records.
Training requirements vary based on user count, technical proficiency, and workflow complexity. Organizations with computer-savvy staff typically require less training time and expense than those with users requiring extensive technical education.
| Cost Factor | Impact Level | Typical Range | Key Considerations |
| Organization Size | High | 1-500+ providers | Primary cost driver |
| Customization | High | $10,000-$500,000+ | Specialty workflows increase costs |
| Integration Complexity | Medium-High | $5,000-$200,000+ | Number of systems to connect |
| Data Migration | Medium | $2,000-$100,000+ | Data quality and volume |
| Training Requirements | Medium | $1,000-$50,000+ | User technical proficiency |
8. How to Optimize the Cost of Implementing EHR
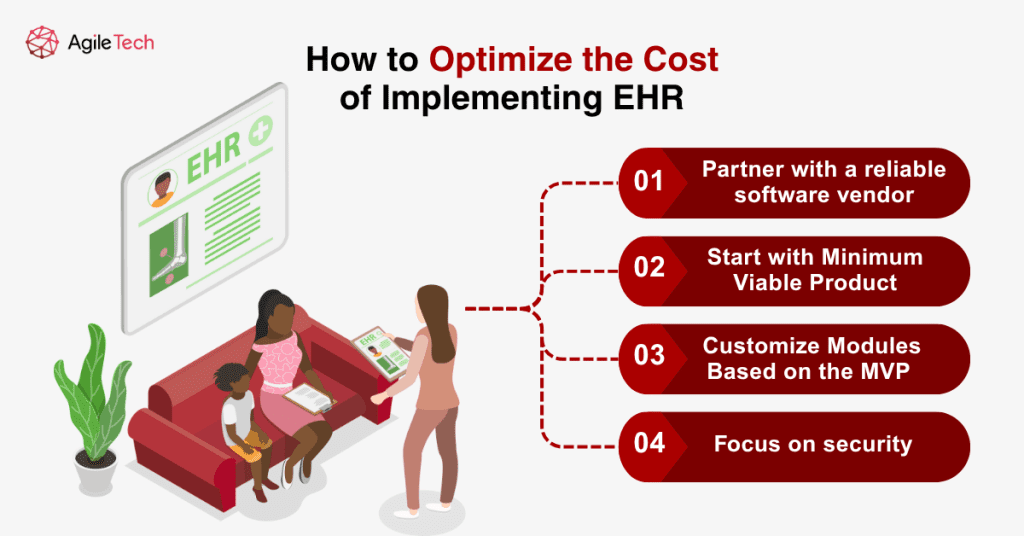
8.1. Partner with a Reliable Software Vendor
Selecting a reliable software vendor represents one of the most critical decisions affecting long-term EHR costs and success. Established vendors with proven track records typically provide more stable platforms, better support services, and predictable upgrade paths. Organizations should evaluate vendor financial stability, customer satisfaction ratings, and long-term strategic direction. Reliable vendors offer comprehensive support services, training programs, and implementation assistance that reduce overall project risk and costs. They typically provide better documentation, user communities, and knowledge resources that help organizations maximize system value. Contract negotiation with reliable vendors often yields better pricing, service level agreements, and flexibility for future needs. Established vendors may offer volume discounts, multi-year pricing guarantees, and favorable terms that reduce long-term costs.
In this context, AgileTech stands out as a trusted partner for healthcare software development. With a highly qualified team of engineers and years of experience in the industry, AgileTech has built a strong reputation for its reliability, technical excellence, and commitment to client success. The company combines deep domain knowledge with proven engineering practices to deliver robust, secure, and scalable healthcare solutions. AgileTech’s focus on transparency, collaboration, and long-term value makes it a dependable choice for organizations seeking to implement or optimize healthcare technologies.
8.2. Start with Minimum Viable Product
Implementing a minimum viable product (MVP) approach helps organizations control costs while achieving core functionality quickly. This strategy focuses on essential features needed for basic operations, deferring advanced capabilities until after successful initial deployment.
MVP implementations typically cost 40-60% less than comprehensive deployments while providing immediate value and user experience. Organizations can evaluate system performance, user satisfaction, and workflow effectiveness before investing in additional features or customization.
This approach reduces implementation complexity, training requirements, and change management challenges. Users can adapt to core functionality before learning advanced features, improving adoption rates and user satisfaction.
8.3. Customize Modules Based on the MVP
After a successful MVP deployment, organizations can systematically add modules and customization based on demonstrated needs and user feedback. This phased approach allows for better budget planning and risk management while ensuring each addition provides clear value.
Module prioritization should focus on features that provide the highest return on investment or address the most significant operational challenges. Organizations can evaluate each module’s cost-benefit ratio before implementation, ensuring optimal resource allocation.
Phased customization allows organizations to learn from initial implementation experiences and apply lessons learned to subsequent phases. This typically results in more efficient implementations and better user satisfaction.
8.4. Focus on Security
Security investment represents a critical cost optimization strategy because security breaches can result in massive financial penalties, reputation damage, and operational disruption. Proactive security investment typically costs far less than reactive breach response and remediation.
Comprehensive security planning should include access controls, data encryption, audit trails, and staff training programs. Organizations should budget for security infrastructure, monitoring tools, and compliance management systems from the beginning of EHR implementation.
Regular security assessments, penetration testing, and vulnerability management help organizations identify and address security gaps before they become expensive problems. This proactive approach reduces long-term risk and compliance costs.
| Optimization Strategy | Cost Reduction Potential | Implementation Difficulty | Timeline | Key Benefits |
| Reliable Vendor Partnership | 20-30% | Low | Immediate | Better support, predictable costs |
| MVP Approach | 40-60% | Medium | 3-6 months | Faster ROI, reduced complexity |
| Phased Customization | 25-40% | Medium | 6-12 months | Better budget control, learned improvements |
| Proactive Security Focus | 15-25% | Low-Medium | Ongoing | Avoid breach costs, compliance assurance |
At AgileTech, we emphasize security, particularly when it comes to creating healthcare solutions. Our healthcare initiatives are created to comply with the highest safety and regulatory standards.
Conclusion
EHR implementation represents a significant investment extending beyond initial software costs. Understanding comprehensive cost structures, including direct expenses, hidden fees, and ongoing operational costs, is essential for successful EHR selection and implementation. The key to successful cost management lies in thorough planning, realistic budgeting, and phased implementation strategies that minimize risk while maximizing value.
As the EHR market continues evolving, organizations should stay informed about pricing trends and best practices that optimize investments. Successful EHR implementation requires balancing cost considerations with functionality needs, ensuring organizations achieve clinical and business objectives while maintaining financial sustainability.