How to Build EHR Systems: Guide to EHR Software Development
What is EHR software, and how do you build one? In this comprehensive guide, we break down everything you need to know about EHR system development, from must-have features to the technologies involved, estimated costs, and why custom EHR software is transforming modern healthcare. With the rise of digital transformation and increasing demand for patient-centered care, electronic health records are more vital than ever. Whether you’re planning to build an EMR app for a private clinic or develop a scalable EHR platform for a hospital network, this article will help you make informed decisions. Read on to explore the full scope of EHR development, its benefits, implementation steps, and how to stay compliant in a regulated industry.
1. What Is EHR Software and How Does It Work?
1.1. What Is EHR Software?
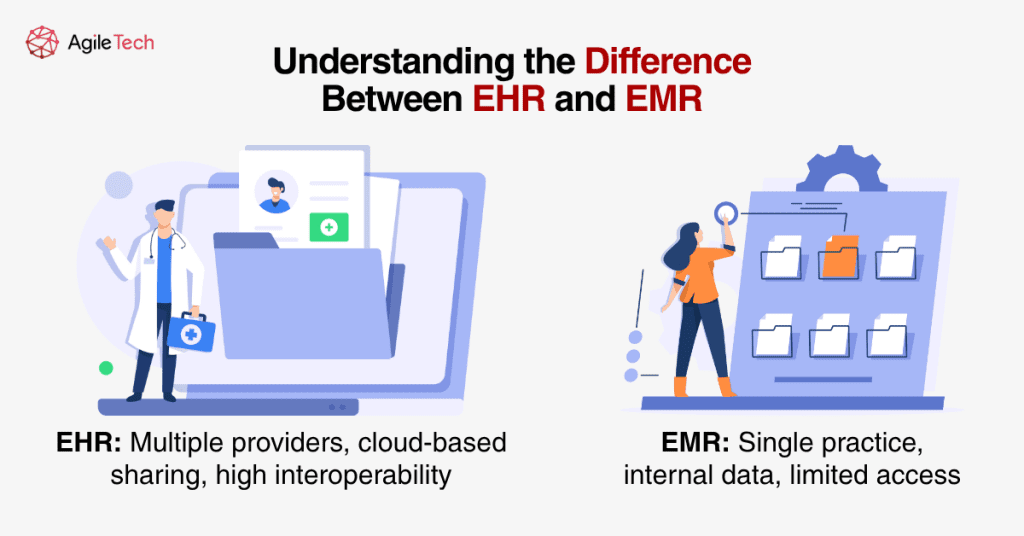
EHR software, or Electronic Health Record software, is a digital platform that centralizes a patient’s medical history, treatment plans, lab results, and more. Unlike EMRs, which are used within a single practice, EHR systems allow for data sharing across multiple healthcare providers. This enables greater collaboration, continuity of care, and reduced medical errors across the healthcare ecosystem. EHR software development focuses on making patient data easily accessible, accurate, and secure for authorized users.
EHR software’s primary aim is to streamline healthcare operations, minimize paperwork, and ensure high-quality patient care. It serves as a single source of truth for patient data, supporting doctors, nurses, pharmacists, and insurance providers in making better decisions. With digitized records, medical professionals save valuable time, leading to quicker diagnoses and improved treatment plans.
Read more: EHR Integration: Step-by-step Guidelines for Healthcare Businesses
1.2. Why EHR Software Matters in Modern Healthcare
EHR systems play a critical role in the digital transformation of healthcare. By digitizing patient records, these platforms streamline administrative tasks, reduce paperwork, and improve patient outcomes. They also help with regulatory compliance by maintaining complete, traceable documentation. EHRs allow healthcare providers to track treatments over time, detect problems early, and provide better patient education. As a result, custom software for EHR has become essential in supporting quality of care, operational efficiency, and legal standards.
Beyond operations, EHR platforms enable personalized medicine. By analyzing historical records and family history, clinicians can tailor treatments to individual needs. Moreover, as global health systems become more integrated, EHR platforms enable cross-border collaboration, especially in areas like telehealth and medical tourism.
1.3. Who Uses EHR Systems?
EHR systems are used by hospitals, private clinics, specialty care centers, and even telehealth providers. They are critical tools for general practitioners, nurses, pharmacists, and administrative staff. From chronic care management to urgent care visits, EHR software development ensures all stakeholders can access accurate, real-time information.
Healthcare payers like insurance companies and government bodies also use EHR data to evaluate quality metrics, reimbursement eligibility, and population health analytics. Meanwhile, researchers leverage EHR databases for clinical trials, public health studies, and evidence-based policy making. These diverse users make interoperability and compliance essential in any EHR system.
2. Core Features of an Effective EHR System
2.1. Must-Have Features
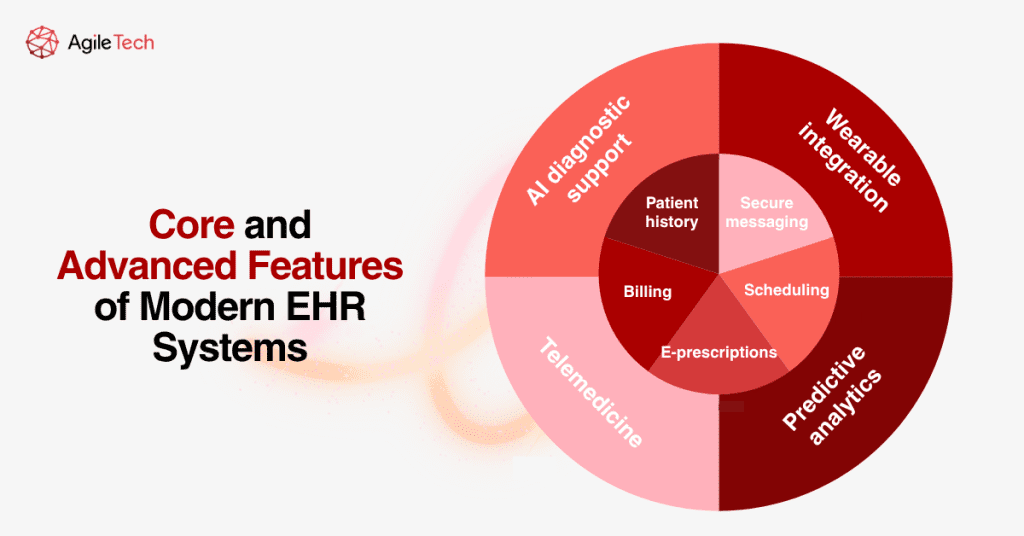
To build an effective EHR system, developers must prioritize features such as medical history tracking, e-prescriptions, appointment scheduling, and billing management. These functionalities not only support clinical decision-making but also improve operational workflows. Patient communication tools, including secure messaging and automated reminders, improve engagement and reduce no-shows. Other essential features include clinical documentation tools, lab result access, and medication reconciliation, which collectively form the foundation of any robust EHR platform.
A well-rounded EHR system should also support task automation. Features like real-time alerts, refill requests, and auto-populated forms increase staff efficiency and reduce administrative burdens. Role-based dashboards allow each user, whether physician, nurse, or receptionist, to access relevant data while protecting patient privacy.
2.2. Advanced Functionalities
Modern EHR software development often includes AI-powered decision support to assist doctors in diagnosis and treatment plans. Natural language processing (NLP) allows voice-to-text dictation and structured clinical notes. Integration with wearable devices and telemedicine platforms further enhances patient monitoring and remote consultations. Predictive analytics can flag high-risk patients or alert physicians to potential complications. These advanced capabilities make the EHR system development more future-proof and competitive.
For example, AI can recommend drug dosages based on a patient’s vitals, history, and genetic profile. Telehealth integration allows clinicians to conduct video visits, prescribe medications, and document encounters in real time. Remote patient monitoring through IoT wearables feeds continuous data into the EHR, offering unprecedented insight into health patterns.
Read more: AI Automation in Healthcare: From Hype to Real-World Applications
2.3. Security & Compliance
Compliance with standards such as HIPAA, HL7, FHIR, and GDPR is non-negotiable when you build an EHR system. Security measures like end-to-end encryption, strict access control, and audit logs protect sensitive data from unauthorized access. Data backup, disaster recovery protocols, and multi-factor authentication are also key components. Healthcare organizations must partner with experienced teams to ensure regulatory adherence and implement ongoing compliance monitoring throughout EHR development.
A successful EHR platform must also support data residency laws where applicable. For instance, GDPR may require data to be stored within the EU. Regular penetration testing, vulnerability scans, and staff training ensure long-term security. Compliance is not a one-time task but a continuous part of system lifecycle management.
3. Types of EHR Systems and Deployment Options
3.1. Cloud-Based vs On-Premise
When choosing an EHR platform, deployment type is key. Cloud-based EHR systems offer scalability, cost-efficiency, and remote access. They are ideal for clinics that want flexibility without heavy infrastructure investment. Cloud providers often include built-in security and compliance features, reducing development overhead. On-premise solutions provide greater data control and may suit larger hospitals with strict data governance needs. These require internal IT teams for server management and software updates. Both options influence EHR software development strategies and long-term cost implications.
| Criteria | Cloud-Based | On-Premise |
| Scalability | High | Medium |
| Initial Cost | Low | High |
| Data Control | Medium | High |
Cloud-based solutions are often subscription-based, which helps smaller clinics control costs early on. They also simplify collaboration and access across multiple locations. However, concerns over internet reliability, vendor lock-in, and ongoing operational costs should be considered. On the other hand, on-premise deployment offers maximum control, particularly for hospitals with strict policies or in locations with limited internet access.
3.2. Open-Source vs Proprietary vs Custom Solutions
Open-source EHR systems are budget-friendly and flexible but may lack full support and documentation. Proprietary software offers vendor support and tested reliability, though customization can be limited. On the other hand, custom EHR development provides full control over features, UI, and integration. You can develop modules tailored to your workflows, ensuring better alignment with your clinical and administrative needs. The right choice depends on your budget, timeline, scalability goals, and internal IT capacity.
Open-source options like OpenMRS or GNU Health allow organizations to build on community-tested frameworks, reducing time to market. However, they typically require strong internal development resources. Proprietary solutions may be ready to deploy faster, but can result in vendor lock-in, rigid pricing models, or misalignment with unique workflows. Custom development balances flexibility and cost by delivering exactly what your organization needs, though it requires more planning and expert collaboration.
3.3. Multi-Tenant vs Single-Tenant Platforms
Multi-tenant platforms share resources among multiple clients, reducing costs and easing updates. SaaS EHR vendors often use these and are easier to maintain centrally. Single-tenant platforms dedicate infrastructure to one client, enhancing data isolation and security, preferred by large hospitals and specialty networks with unique security needs. Each architecture has trade-offs in terms of cost, speed, and customization. EHR system development should align with your institution’s structure, growth plans, and risk tolerance.
Multi-tenancy is ideal for small to mid-sized clinics that don’t require full isolation and prefer lower operational costs. Updates can be rolled out universally without manual intervention. In contrast, single-tenant systems offer full control over customizations and upgrades, making them more suitable for large networks handling sensitive patient data across departments.
4. Step-by-Step Guide: How to Build an EHR System
| Phase | Timeline | Description |
| Step 1: Requirements | Week 1–2 | Define goals |
| Step 2: UX/UI Design | Week 2–4 | Build wireframes |
| Step 3: Choose Tech Stack | Week 4–5 | Select frameworks |
| Step 4: MVP | Week 8–16 | First usable version |
| Step 5: Compliance Testing | Week 16–18 | HIPAA & Security checks |
| Step 6: Launch & Integrate | Week 18–20 | Roll out and link systems |
| Step 7: Maintenance | Ongoing | Updates & scaling |
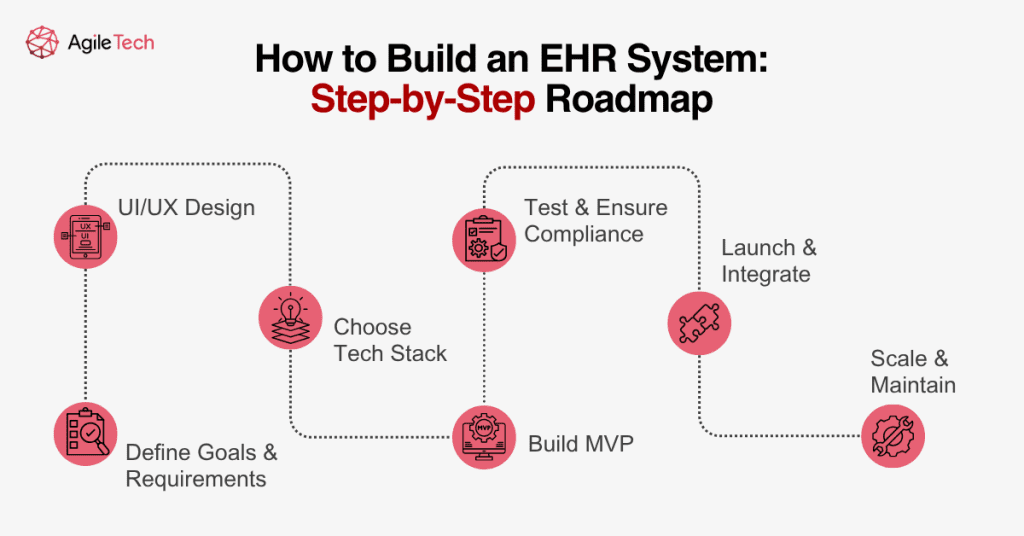
Step 1: Define Goals and Requirements
Every successful EHR system starts with a well-defined purpose. Begin by identifying your target users: doctors, nurses, patients, or administrators, and map out their needs. List key functionalities you expect, such as lab integration, billing, or telehealth modules. Set clear compliance requirements based on your region (e.g., HIPAA, GDPR). These foundational steps ensure the EHR software development aligns with both user expectations and legal obligations.
Stakeholder interviews and workflow mapping are useful tools at this stage. Involving end users early improves adoption later. Requirements gathering should also consider localization, scalability, and mobile accessibility.
Step 2: UX/UI Design and User Journey
User experience plays a major role in adoption. Design interfaces that are intuitive, responsive, and role-specific. For example, physicians might need quick access to patient history and lab results, while front-desk staff focus on appointment scheduling. Wireframes, user flow maps, and prototype testing are essential in this phase. Consistent feedback loops with stakeholders ensure that the EHR platform meets real-world usability standards.
Great UI/UX design reduces training time, improves accuracy, and increases staff satisfaction. Design thinking sessions with diverse users, doctors, nurses, and receptionists help identify edge cases and friction points before development.
Step 3: Choose Tech Stack
The tech stack determines how secure, scalable, and efficient your system will be. Most backend systems rely on Java, Python, or Node.js, while front-end interfaces are built with React, Angular, or Vue.js. For databases, consider PostgreSQL or MongoDB. Cloud infrastructure providers like AWS, Azure, or GCP offer robust scalability and security. Ensure your stack includes libraries or tools that support healthcare standards such as HL7 or FHIR.
It’s critical to evaluate vendor lock-in, compliance readiness, and integration options when selecting technologies. Make sure your stack also supports RESTful APIs or GraphQL for future expansion and interoperability.
Step 4: Develop an MVP
Rather than build the entire EHR system at once, start with a Minimum Viable Product. Focus on critical modules such as electronic records, patient registration, appointment scheduling, and e-prescribing. MVPs allow you to launch faster, collect feedback, and iterate effectively. This also helps control costs and align development with actual user needs.
Development teams should follow Agile methodology, with two-week sprints and regular stakeholder demos. Feature flags can be used to test features incrementally without affecting the core system.
Step 5: Test and Ensure Compliance
Testing is more than finding bugs; it ensures patient safety, data integrity, and legal adherence. Conduct functional testing, performance testing, and usability testing under real-world conditions. Use automated tools where possible, but include manual testing for workflows. Validate data security, access rights, and encryption standards to confirm compliance with HIPAA, HL7, and other protocols.
Include test scenarios for common use cases, such as medication refills or patient discharge, to assess real-world readiness. Compliance testing should be documented and reviewed by legal or IT audit teams.
Step 6: Launch and Integrate
Plan a soft launch with limited users before full-scale deployment. Monitor usage, gather insights, and fix issues early. Integration with third-party systems like pharmacies, diagnostic labs, payment processors, and existing hospital software must be seamless. Use APIs and standardized protocols to enable smooth data exchange across platforms.
Prepare detailed integration documentation for partners, and schedule downtime in advance to minimize clinical disruptions. Ensure training materials and user support are ready before go-live.
Step 7: Scale and Maintain
After go-live, continuous monitoring, user training, and feature updates are necessary. Establish a maintenance plan covering software patches, backups, uptime monitoring, and user support. Use analytics tools to measure performance and identify bottlenecks. A successful EHR platform evolves with changing user needs and regulatory requirements.
Post-launch support should include tiered helpdesk levels, detailed SLAs, and automated incident reporting. Monthly or quarterly review cycles can drive long-term improvement.
5. How Much Does It Cost to Build an EHR System?
5.1. Major Cost Drivers
The cost of building an EHR system varies significantly depending on multiple factors. Custom development from scratch tends to be more expensive than using pre-built templates or open-source frameworks. The more features and integrations required, the higher the complexity and cost. Location of the development team is another key driver: hiring developers in the U.S. or Western Europe typically costs 2–3 times more than working with offshore teams in Vietnam, India, or Eastern Europe. In addition, regulatory requirements, data storage infrastructure, and integration with third-party services (e.g., pharmacy systems, labs, payment gateways) can all add substantial costs to your EHR software development budget.
Another factor that influences cost is the timeline. Projects with tight deadlines often require more resources to deliver on time, leading to higher hourly costs. Moreover, technical debt can accumulate if corners are cut in initial development stages to reduce costs, resulting in larger long-term maintenance expenses. It’s also worth noting that healthcare-specific certifications for developers or consultants (e.g., HIPAA-certified consultants) can command higher rates.
5.2. Development Budget Estimates
Budget planning should consider both short- and long-term needs. An MVP for an EMR or EHR system with limited features may cost between $40,000 and $80,000. This typically includes basic modules like patient registration, clinical notes, appointment scheduling, and e-prescriptions. A full-scale custom EHR platform with advanced functionality, telemedicine, AI diagnostics, wearable integration, and multi-role dashboards can cost anywhere from $100,000 to over $250,000. Projects for large hospitals and healthcare networks may even exceed $500,000 due to the complexity of workflows, user types, and integration layers.
Budgeting should include not only development time but also testing, security audits, deployment, onboarding, and training. Depending on the provider’s goals, the budget may also need to account for mobile apps (iOS/Android), admin portals, and data migration from legacy systems. For example, migrating data from outdated EMR platforms can cost thousands of dollars alone if not automated efficiently.
5.3. Ongoing Costs Post-Launch
Once launched, an EHR platform incurs ongoing operational and maintenance costs. These include monthly cloud hosting fees, user support services, and compliance updates. You’ll need to allocate a budget for periodic upgrades, bug fixes, performance optimization, and backups. Security enhancements, including penetration testing and system audits, are essential to protect patient data and ensure HIPAA or GDPR compliance. For enterprise-level EHR systems, annual maintenance can range from 15–25% of the initial development cost.
In addition, operational costs can scale as your practice grows. As more users access the system and data volumes increase, you may need to expand storage, increase processing power, or upgrade third-party services. Regular staff training and onboarding of new users should also be part of your post-launch investment plan.
5.4. How to Optimize Costs Without Sacrificing Quality
There are several ways to manage costs while still delivering a robust EHR platform. First, start with an MVP to test market fit and gather feedback. Second, leverage open-source tools and libraries, such as OpenMRS or LibreHealth, which provide base functionality and reduce time-to-market. Third, consider hiring an offshore development team with proven healthcare experience and clear deliverables. Define a precise scope of work (SOW) and avoid feature creep during development. Finally, use modular architecture so you can scale or enhance the system in stages rather than building everything up front.
Organizations can also explore hybrid approaches, combining proprietary components with open-source modules to reduce time and cost without giving up functionality. Additionally, using low-code or no-code platforms for non-critical admin features (e.g., patient satisfaction surveys) can reduce frontend development time.
6. Why Invest in Custom EHR Software?
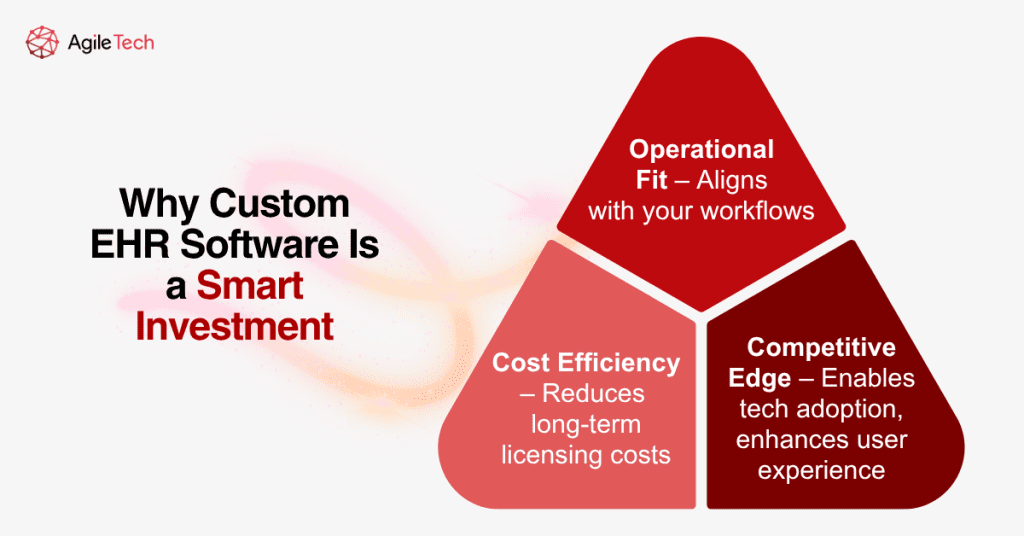
6.1. Addressing Unique Operational Needs
Every healthcare provider operates under different rules, policies, and care delivery models. Off-the-shelf solutions often lack the flexibility to match these unique operational needs. Custom EHR software allows organizations to build workflows that reflect their actual processes, not the other way around. Whether it’s integrating with a legacy lab system, accommodating multi-language support, or creating specialized templates for different departments, custom EHR development ensures adaptability and alignment. It also offers the ability to incorporate user feedback directly into future versions.
For example, a mental health provider may need a completely different intake form and medication tracking flow than an urgent care clinic. Custom systems also allow integration with in-house analytics tools, internal APIs, or government e-health platforms, offering a seamless workflow that generic systems simply cannot.
6.2. Long-Term Cost Efficiency
While upfront investment may be higher for custom software, the long-term benefits outweigh the initial costs. With a tailored EHR platform, healthcare providers avoid costly licensing fees and third-party platform dependencies. This independence allows for ongoing improvements without incurring additional charges or waiting for vendor updates. Moreover, custom systems can be designed for scalability, helping healthcare organizations grow without switching systems later. Over time, this results in lower total cost of ownership (TCO).
Organizations also gain control over their roadmap, update cycles, and feature prioritization, something not typically possible with commercial off-the-shelf software (COTS). The ability to optimize performance, data usage, and UX over time brings not only cost savings but operational resilience.
6.3. Gaining a Competitive Edge in Healthcare
Custom EHR solutions provide a strategic advantage in today’s competitive healthcare landscape. With a platform designed to your specifications, you can create seamless, branded digital experiences for patients and providers. Advanced features like predictive analytics, AI-supported diagnostics, and personalized health dashboards improve both operational decision-making and patient satisfaction. In addition, organizations can experiment with innovation faster, piloting new technologies that distinguish them in the market while also aligning with long-term digital transformation goals.
In a value-based care model, outcomes are as important as efficiency. With custom EHR systems, providers can fine-tune care paths, monitor clinical outcomes, and measure ROI on initiatives such as remote patient monitoring or chronic disease management.
7. A Quick Look at EMR Systems and How They Differ
7.1. What Is EMR Software?
Electronic Medical Records (EMRs) are digital versions of paper charts found in a clinician’s office. EMRs contain a patient’s medical history, diagnosis, treatments, prescriptions, immunizations, and test results, but only within one healthcare organization. Unlike EHR systems, EMRs are not designed to be shared across different facilities or platforms. Their scope is narrow and tailored for single-practice use, making them ideal for independent clinics or solo practitioners.
Despite their limitations, EMRs play an important role in modernizing internal workflows. They allow doctors to search, filter, and update patient data in real time. They often include built-in tools for charting, e-prescribing, and scheduling. However, they do not support multi-location data sharing, making collaboration across networks difficult.
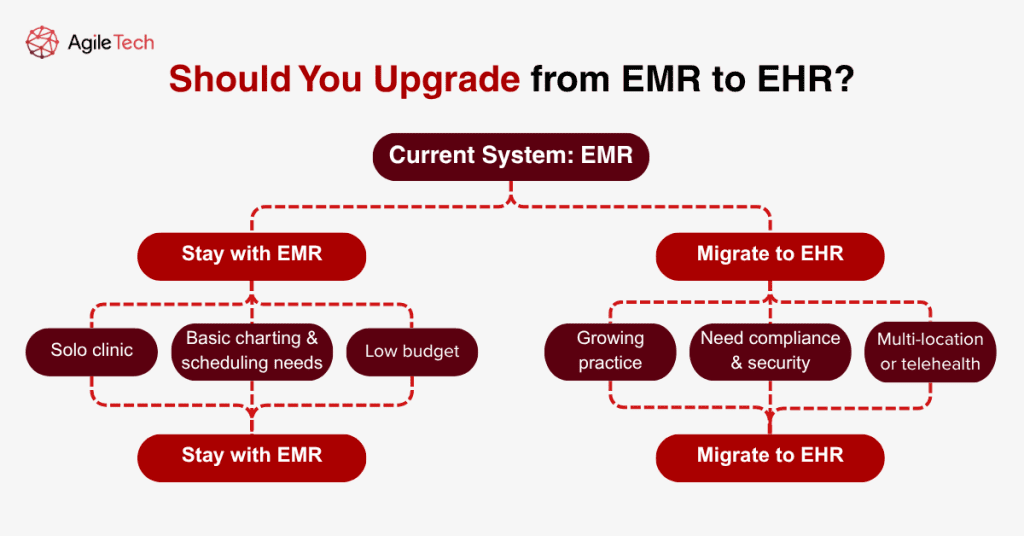
7.2. When to Choose EMR Instead of EHR
For healthcare providers with a single location and a limited scope of services, building an EMR app may be a more cost-effective and simpler alternative. EMR systems offer quick setup, lower development and maintenance costs, and fewer compliance hurdles. They’re especially suited for small practices that focus on routine care, such as dermatology clinics, dental offices, or general outpatient facilities.
However, if your organization plans to grow, join a medical network, or adopt telemedicine features, starting with an EHR or at least a modular EMR that supports future integration is recommended. Transitioning from EMR to EHR later can be complex and costly due to data format inconsistencies and a lack of interoperability.
7.3. EMR to EHR Migration: Is It Worth It?
Migration from EMR to EHR involves converting data formats, standardizing clinical records, and ensuring compliance with broader interoperability standards. While the process can be technically challenging, it is often a strategic move for practices looking to scale, offer remote care, or meet national health record mandates.
Benefits include improved patient safety, better care coordination, enhanced data analytics capabilities, and eligibility for federal reimbursement programs in some countries. Tools like data mapping, middleware connectors, and automated ETL (extract-transform-load) solutions can streamline the migration process.
Conclusion
EHR software development is not just a technical task; it’s a long-term investment in operational efficiency, patient satisfaction, and regulatory compliance. Whether you’re a startup clinic or a large hospital system, understanding how to build an EHR system properly helps you avoid common pitfalls and make smarter strategic decisions.
At AgileTech Vietnam, we specialize in building custom EHR and EMR platforms that are scalable, secure, and user-centric. Our team brings deep expertise in healthcare software, compliance, and modern tech stacks. Let us help you create a digital solution tailored to your clinical goals.