Telemedicine Software Development: Types, Benefits, and How to Build It Right?
Telemedicine is reshaping the healthcare experience, making care more accessible, efficient, and patient-focused. As demand grows, many providers and startups are turning to telemedicine software development to deliver secure and scalable digital health solutions. From real-time consultations to remote monitoring, telehealth software development enables clinics and hospitals to stay ahead. This blog breaks down the key types, benefits, and how to build the best telemedicine software with the right telemedicine software provider or telemedicine software development company. If you’re planning to launch or upgrade a telehealth software system, this guide is your starting point.
- 1. What Is Telemedicine Software?
- 2. Types of Telemedicine Software Solutions
- 3. How to Choose the Right Partner for Your Telehealth Platform
- 4. What are the Benefits of Telemedicine Software?
- 5. The Telemedicine Software Development Process
- 6. Challenges of Telemedicine Software Development
- 7. How Much Does Telemedicine Software Cost?
- 8. AgileTech's Telemedicine Software Development Services
- Conclusion
- FAQs
1. What Is Telemedicine Software?
Telemedicine software is a digital platform that enables healthcare providers to deliver medical services remotely through secure video calls, messaging, data sharing, and real-time patient monitoring. These systems are designed to improve access to care, reduce operational costs, and enhance patient engagement, especially in rural or underserved areas.
In the context of telemedicine software development, the goal is to build HIPAA-compliant, scalable, and user-friendly solutions that support a wide range of use cases—from general consultations and mental health services to chronic disease management and post-op follow-ups.
A robust telehealth software system typically includes features such as appointment scheduling, electronic health records (EHR) integration, digital prescriptions, payment processing, and analytics dashboards for both patients and providers.
Technologies used in telemedicine
Successful telemedicine software development depends on integrating the right technologies to ensure security, scalability, and a smooth user experience. Today’s leading telehealth software systems are powered by a combination of tools that enable real-time care, data security, and system flexibility.
Key technologies include:
- Video conferencing APIs (e.g., WebRTC, Twilio) for secure, real-time doctor-patient communication
- Cloud infrastructure for flexible data storage and remote access
- EHR integration to sync patient data across healthcare systems
- AI and machine learning for triage automation, predictive care, and symptom analysis
- IoT devices to support real-time remote monitoring of patient vitals
- Mobile-first frameworks like Flutter or React Native for responsive cross-device access
- Cybersecurity measures such as end-to-end encryption and multi-factor authentication to meet HIPAA or GDPR standards
Together, these tools form the backbone of software telemedicine, enabling healthcare providers and telemedicine software development companies to deliver reliable, compliant, and scalable virtual care solutions.
2. Types of Telemedicine Software Solutions
Not all telemedicine software solutions serve the same purpose. Depending on your medical services, target users, and operational model, different platforms address different needs, from real-time consultations to chronic care monitoring. That’s why defining the right telehealth software system early in your telemedicine software development process is essential to success.
Here are the most common types of software telemedicine solutions used today:
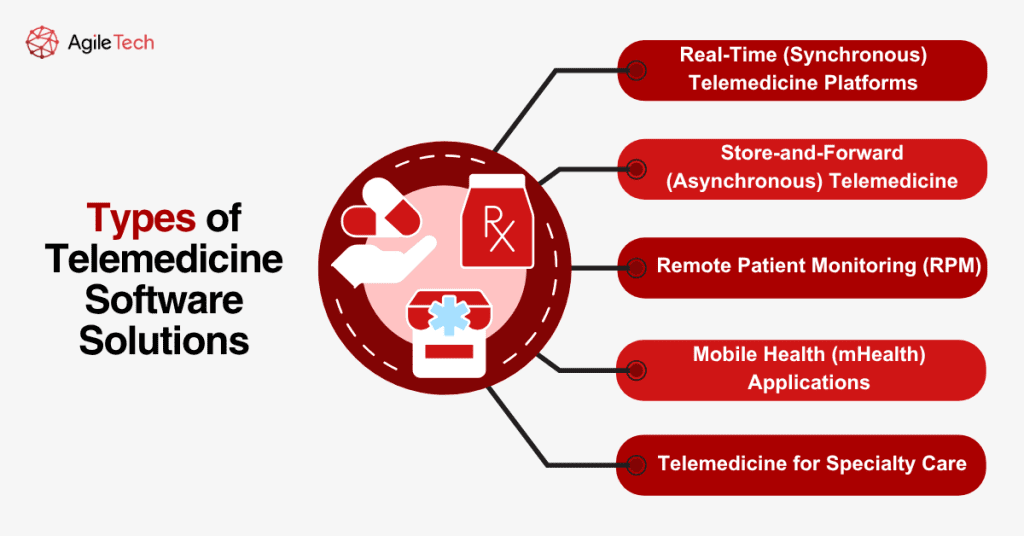
2.1. Real-Time (Synchronous) Telemedicine Platforms
These platforms enable live video or audio consultations between healthcare providers and patients. They are widely used for virtual primary care visits, urgent care, follow-up appointments, and mental health therapy. A solid telemedicine software provider will prioritize low-latency communication, secure video conferencing APIs (e.g., WebRTC), and features like appointment scheduling and e-prescriptions. Real-time systems improve accessibility, reduce wait times, and offer immediate interaction between patient and clinician.
2.2. Store-and-Forward (Asynchronous) Telemedicine
This model allows medical data, like lab results, images, or patient histories, to be securely uploaded and reviewed later by a specialist. Commonly used in fields like dermatology, radiology, and pathology, it removes the need for both parties to be present at the same time. For a telemedicine software development company, building this system involves robust backend infrastructure, file encryption, and audit tracking for compliance.
2.3. Remote Patient Monitoring (RPM)
RPM systems are ideal for managing chronic conditions or post-operative care. Patients use connected devices (e.g., blood pressure monitors, glucose meters, or wearable ECGs) to transmit real-time data to healthcare providers. This continuous stream of health metrics supports early detection, timely interventions, and long-term care strategies. Developing an RPM-focused telehealth software system requires expertise in IoT integration, secure cloud environments, and real-time data processing.
2.4. Mobile Health (mHealth) Applications
mHealth apps run on smartphones and tablets, offering a portable, user-friendly way for patients to manage their health. These apps commonly support features like virtual consultation booking, symptom checkers, medication reminders, and health record access. mHealth plays a big role in telemedicine software development services, especially for startups or outpatient clinics looking to expand reach and engagement on a budget.
2.5. Telemedicine for Specialty Care
These platforms are custom-built for specific medical fields such as telepsychiatry, teledermatology, or telecardiology. Each requires domain-specific features—for example, mood-tracking tools for psychiatry or high-resolution image upload for dermatology. A niche-specific telemedicine software development company ensures these platforms reflect the actual workflows of specialists, enhancing accuracy and user satisfaction.
3. How to Choose the Right Partner for Your Telehealth Platform
The success of your telehealth initiative depends not only on the idea itself, but also on who builds it with you. Selecting the right telemedicine software development company is one of the most strategic decisions that can define the reliability, security, and scalability of your entire digital health platform. In an increasingly crowded market, making the wrong choice could lead to compliance issues, technical debt, or poor user adoption.
To find a partner who can help you build a sustainable and secure teleh
ealth software system, consider the following key aspects:
3.1. Healthcare-Specific Experience
Your chosen telemedicine software provider should have proven experience working with healthcare organizations. Look for portfolios or case studies that involve hospital systems, clinics, or wellness startups. A vendor that understands the nuances of clinical workflows, digital health records, and patient engagement will deliver faster and more aligned results.
3.2. Security & Regulatory Compliance
Security isn’t optional, it’s foundational. The partner must be proficient in building HIPAA-compliant systems (for the US), GDPR-ready platforms (for the EU), or local standards like ISO 13485 or MOH requirements. Patient data encryption, role-based access, and audit trails should be part of their telemedicine software development services by default.
3.3. Customization Capabilities
Off-the-shelf solutions rarely satisfy all business needs. A reliable vendor should offer flexible development options, allowing you to design workflows, dashboards, and integrations specific to your organization’s goals. Whether you’re building an AI-powered triage assistant or a remote patient monitoring app, the right partner will tailor the solution to fit.
3.4. Full-Cycle Technical Support
Beyond initial development, long-term support is vital. Choose a vendor offering end-to-end services: from discovery and UX/UI design to deployment, maintenance, and future upgrades. A full-cycle telemedicine software development company can help you evolve the product with new features and respond quickly to industry changes.
3.5. Technology Expertise & Innovation
Ask about their tech stack and innovation culture. Do they use modern frameworks? Are they integrating machine learning, IoT devices, or blockchain in their solutions? A tech-savvy partner will help you stay ahead of the curve in an evolving digital health landscape.
3.6. Reputation & Client Feedback
Don’t just rely on sales decks—check third-party platforms like Clutch, G2, and GoodFirms for authentic client reviews. Read testimonials on transparency, delivery timelines, communication, and responsiveness. A trusted telemedicine software provider will have a consistent record of satisfied healthcare clients.
Choosing a partner with both domain experience and technical agility ensures your platform won’t just function—it will thrive. That’s why many healthcare organizations partner with firms like AgileTech, whose experience in telemedicine software development services spans multiple regions and includes scalable, compliant, and user-centric solutions tailored to modern healthcare demands.
4. What are the Benefits of Telemedicine Software?
Telemedicine software offers valuable advantages to patients, physicians, and healthcare organizations alike. Its ability to enhance access and streamline the delivery of care makes it a compelling reason for many to invest in telehealth software development. Below, we explore the key benefits that each stakeholder can gain from adopting telemedicine solutions.
4.1. Benefits for Patients
Improved Access to Healthcare
Telemedicine breaks down geographic barriers. According to the CDC, 80% of adults in the U.S. have used telemedicine at least once, showing how virtual care is becoming mainstream, especially for those in rural or underserved areas.
High Patient Satisfaction
Remote consultations provide convenience and comfort. According to Eagle Telemedicine, 87% of patients were either satisfied or very satisfied with their telehealth experience, reinforcing its credibility as an effective care delivery model.
Increased Convenience and Time Savings
Patients can consult doctors without leaving home, avoiding travel and reducing wait times. A Doximity report shows that 88% of users believe telemedicine improves access to care, especially for those with mobility limitations or tight schedules.
4.2. Benefits for Healthcare Providers
Increased Revenue and Cost Savings
Video meetings are more time- and cost-efficient than in-person visits. According to Stream, 53% of healthcare systems report that telemedicine lowers operational costs, indicating a positive impact on financial performance through reduced overhead, fewer facility needs, and optimized staffing.
Wider Patient Reach
Telehealth allows providers to serve patients beyond physical locations. With remote consultations, hospitals can offer 24/7 service, improve patient acquisition, and grow their market. The global telemedicine market is projected to reach $451.4 billion by 2032, growing at a CAGR of 18.3% (Allied Market Research).
Data-Driven Clinical Efficiency
Modern telehealth platforms often come with built-in analytics and reporting tools, helping healthcare providers track performance, identify patient trends, and improve operational efficiency.
4.3. Benefits for Doctors
Greater Work-Life Flexibility
Telemedicine empowers doctors to practice from anywhere, helping them better balance workloads and reduce burnout. Flexible scheduling leads to higher productivity and job satisfaction.
More Efficient Workflows
With telehealth tools, doctors can manage appointments, review patient data, and handle documentation seamlessly in one place, saving time and reducing admin burden. The CDC reports that over 73% of specialty physicians acknowledge equal or better outcomes through telemedicine.
Stronger Patient Relationships
Frequent touchpoints made possible by virtual care improve follow-ups, medication adherence, and chronic care management, leading to deeper engagement and better clinical outcomes.
5. The Telemedicine Software Development Process
Building a successful telemedicine platform requires more than just a great idea, it involves a well-structured, multi-phase approach that ensures regulatory compliance, seamless functionality, and a great user experience. Whether you are a startup launching a niche app or a hospital system digitizing services, partnering with a trusted telemedicine software development company is essential for success.
Here’s a step-by-step guide to the telemedicine software development process, designed to help you understand what it takes to create a secure and scalable telehealth software system.
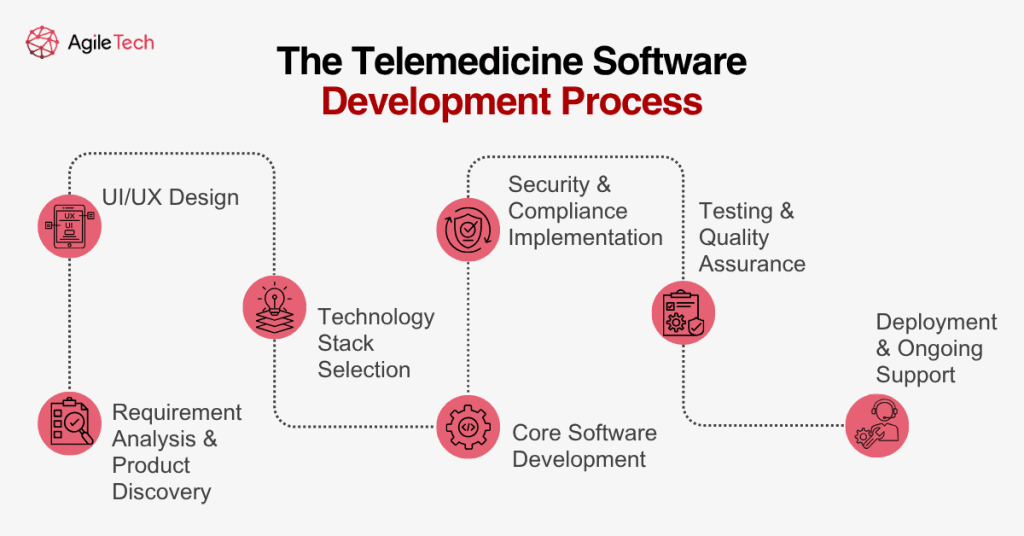
5.1. Requirement Analysis & Product Discovery
Every successful telehealth platform starts with a deep understanding of its users and market. In this phase, stakeholders define core functionalities, patient needs, doctor workflows, and local healthcare regulations (HIPAA, GDPR, etc.). An experienced telemedicine software provider will guide you through technical feasibility assessments and help prioritize must-have features like video consultations, digital prescriptions, and EMR integration.
5.2. UI/UX Design
A seamless user experience is crucial in healthcare applications. This step focuses on designing intuitive dashboards for both patients and practitioners. Designers ensure the telemedicine software is mobile-responsive, accessible for different user groups (including elderly patients), and optimized for low-bandwidth environments when needed.
5.3. Technology Stack Selection
The choice of technology impacts system performance, scalability, and long-term cost. A trusted telemedicine software development company like AgileTech helps businesses select secure and modern tech stacks, including:
- Video conferencing APIs (e.g., WebRTC, Agora)
- Backend frameworks (Node.js, Django, Laravel)
- Cloud platforms (AWS, Azure, Google Cloud)
- HIPAA/GDPR-compliant database systems
- Integration with EHR, CRM, or third-party medical APIs
Tailored software telemedicine solutions ensure your system can adapt as your services grow.
5.4. Core Software Development
This is the heart of the process, where development teams begin coding the platform using agile methodologies. Key modules developed during this phase include:
- Encrypted video consultation
- Appointment scheduling & notifications
- Secure patient data storage
- Integrated payment systems
- Role-based access for doctors, patients, and admins
- Real-time messaging
- Digital prescription & medical records
Developers also ensure that the telehealth software development aligns with national healthcare laws and data privacy guidelines.
5.5. Security & Compliance Implementation
Security is non-negotiable. A reliable telemedicine software development company will implement the latest cybersecurity standards, including:
- End-to-end encryption
- Multi-factor authentication
- Role-based user permissions
- Audit logs and data recovery protocols
- Compliance with HIPAA, GDPR, and local Ministry of Health standards
These steps protect both patient confidentiality and institutional credibility.
5.6. Testing & Quality Assurance
Before going live, rigorous QA testing is carried out to validate every feature. This includes:
- Functional testing of all modules
- Performance & load testing
- Security vulnerability scanning
- Usability testing with real users
Thorough testing ensures that the telemedicine software development services result in a product that performs reliably in real-world scenarios.
5.7. Deployment & Ongoing Support
After a successful launch, the platform is deployed on a secure cloud environment or on-premise server. A good telehealth software provider will also offer continuous support and updates to fix bugs, roll out new features, and ensure compliance with evolving regulations.
A structured approach to telemedicine software development not only ensures that your digital health product meets industry standards but also enhances trust and adoption among users. With the right technology partner and a clear roadmap.
6. Challenges of Telemedicine Software Development
Despite the rapid adoption of telehealth solutions worldwide, telemedicine software development presents a unique set of challenges. While the benefits of virtual healthcare are undeniable, ranging from increased patient access to operational efficiency, developing a fully functional, compliant, and scalable telehealth software system requires careful planning and execution. Below are some of the most critical challenges healthcare organizations and telemedicine software providers face during the development lifecycle.
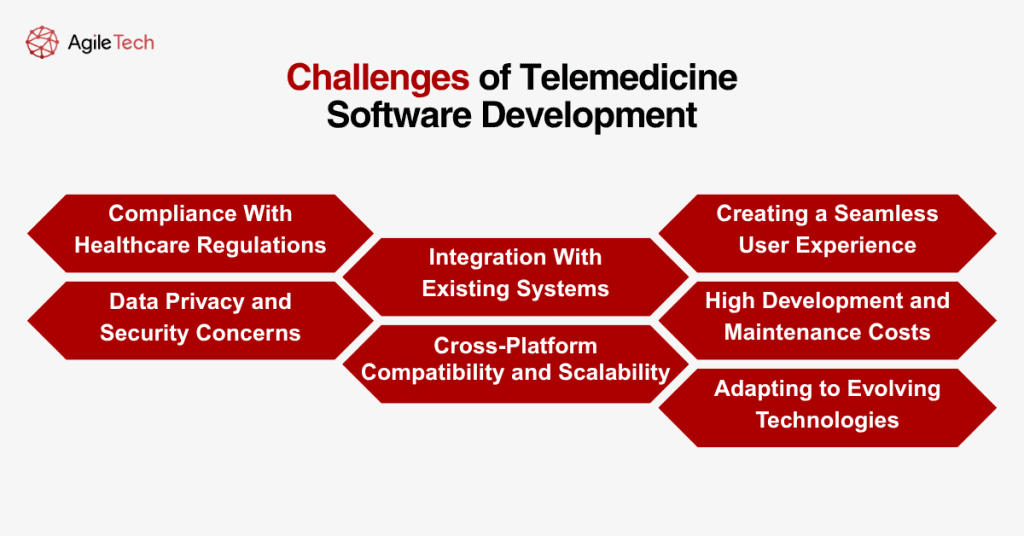
6.1. Compliance With Healthcare Regulations
One of the biggest challenges in building telemedicine platforms is ensuring compliance with strict healthcare regulations. Depending on the target market, developers must consider frameworks like HIPAA (USA), GDPR (EU), PIPEDA (Canada), or region-specific Ministry of Health regulations. These laws dictate how sensitive patient data should be stored, transmitted, and accessed. Failing to meet these requirements can result in costly penalties, legal issues, and reputational damage. Achieving full compliance often involves implementing features such as end-to-end encryption, role-based access control, and secure authentication protocols, which increases the complexity of the development process.
6.2. Data Privacy and Security Concerns
Healthcare data is one of the most targeted types of information for cyberattacks. Building a secure telehealth software system that can protect against breaches, ransomware, and unauthorized access is a top priority. Developers must incorporate robust cybersecurity practices, including secure API connections, encrypted communication, and frequent vulnerability assessments. Security audits and penetration testing must also be a regular part of the development cycle to ensure continued protection post-deployment.
6.3. Integration With Existing Systems
Most healthcare institutions already operate with various digital systems such as EHR (Electronic Health Records), insurance processing platforms, or pharmacy software. A custom telemedicine software development project must be capable of integrating seamlessly with these systems to avoid operational bottlenecks. However, outdated legacy systems, inconsistent data formats, and a lack of API documentation often hinder smooth integration, causing delays and additional costs.
6.4. Cross-Platform Compatibility and Scalability
Modern telehealth software systems must operate smoothly across various devices—desktops, smartphones, tablets—and operating systems. Ensuring cross-platform functionality requires significant testing and UI/UX refinement. Additionally, the system must be scalable to handle increased traffic during peak hours, such as during health crises or seasonal illness spikes. Poor scalability can result in system crashes, delayed consultations, and user dissatisfaction.
6.5. Creating a Seamless User Experience
User experience is critical in the healthcare industry, where patients may not be tech-savvy and doctors need intuitive workflows. A telemedicine software provider must prioritize simplicity and accessibility without compromising functionality. This involves designing easy-to-navigate interfaces, streamlining the onboarding process, and reducing friction in tasks such as scheduling, uploading documents, or initiating video consultations. If users struggle to navigate the system, adoption rates will suffer, no matter how robust the back-end features are.
6.6. High Development and Maintenance Costs
While the cost of telemedicine software development can be optimized through outsourcing or MVP strategies, building a compliant and high-performing solution still requires a significant investment. This includes costs for cybersecurity infrastructure, third-party APIs, UI/UX design, and continuous updates to stay aligned with regulations and user feedback. Maintenance, in particular, is an ongoing challenge as it demands continuous bug fixes, security patches, and performance optimization.
6.7. Adapting to Evolving Technologies
The telehealth landscape is rapidly evolving, with emerging technologies such as AI diagnostics, IoT-based monitoring devices, and wearable integration entering the market. To stay competitive, a telemedicine software development company must continuously innovate and adapt to these technologies. However, integrating such tools adds complexity to the system and demands expertise that not all teams may possess.
7. How Much Does Telemedicine Software Cost?
The cost of implementing telehealth software depends on multiple factors, including the type of solution, feature complexity, UI/UX design, third-party integrations, and the hourly rates of the development team. On average, telemedicine software development can range from $150,000 to over $250,000. However, it’s difficult to provide a precise estimate without first defining the app’s functionality, scope, and development model.
Fortunately, building an in-house team isn’t the only option. Many experienced telemedicine software development companies offer end-to-end services that are both efficient and cost-effective. To help you plan better, we’ve analyzed approximate costs by region and average hourly rates by role. Rates vary significantly depending on location — for instance, developers in North America tend to charge the highest, but higher cost doesn’t always equate to better quality or access to niche tech skills.
| Telemedicine development specification | North America | Latin America | Central Europe | Western Europe | Asia | Africa |
|---|---|---|---|---|---|---|
| Developers | $80-$100 | $35-$70 | $25-$50 | $30-$65 | $20-$45 | $25-$45 |
| UI/UX Designer | $70-$80 | $40-$60 | $35-$45 | $30-$50 | $20-$30 | $20-$30 |
| Project Manager | $70-$80 | $40-$60 | $50-$70 | $30-$50 | $20-$30 | $25-$35 |
| Business Analyst | $60-$75 | $35-$60 | $25-$35 | $25-$45 | $15-$25 | $20-$30 |
| QA Specialist | $60-$75 | $35-$60 | $25-$40 | $25-$45 | $15-$25 | $20-$30 |
| DevOps | $80-$100 | $35-$70 | $30-$50 | $30-$65 | $20-$45 | $25-$45 |
| Web Team Lead | $85-$110 | $45-$80 | $45-$55 | $45-$65 | $35-$45 | $30-$45 |
Central and Eastern Europe, by contrast, has emerged as a preferred destination for telehealth software development outsourcing. The region offers highly skilled developers with competitive rates, typically between $25 and $50 per hour. Partnering with custom telemedicine software providers from this region allows businesses to access top-tier technical expertise, including hard-to-find specializations, while optimizing development budgets. In fact, even major global tech companies like Google regularly rely on outsourcing to scale their products effectively.
8. AgileTech’s Telemedicine Software Development Services
As the demand for digital healthcare continues to rise, AgileTech offers tailored telemedicine software development services that help healthcare organizations transform their patient engagement, streamline operations, and ensure regulatory compliance. With years of experience in telehealth software development, our team delivers custom-built, secure, and scalable solutions that align with your specific medical workflows and business goals.
Whether you’re a hospital, clinic, or healthcare startup, we offer end-to-end telemedicine software development from ideation to deployment, using the latest technologies and industry best practices. AgileTech’s solutions are compliant with global healthcare regulations, including HIPAA, GDPR, and local health authority guidelines, ensuring safe data management and patient privacy.
Our custom telehealth software systems are designed with flexibility and integration in mind. We build platforms that support:
- Encrypted video consultations and real-time communication
- Appointment scheduling and automated reminders
- Integration with EHR/EMR systems and pharmacy APIs
- AI-powered triage and symptom checkers
- Cloud-based scalability and offline access for remote areas
- Payment gateways and digital insurance processing
- Role-based access for doctors, patients, and administrators
As a dedicated telemedicine software development company, we don’t just code; we consult, design, and innovate with you. AgileTech’s approach emphasizes user-friendly design, efficient performance, and adaptability to emerging technologies, including IoT devices and AI tools for diagnostics and monitoring.
If you’re looking for a reliable telemedicine software provider to bring your vision to life, AgileTech is ready to be your long-term partner in digital healthcare innovation.
Conclusion
Telemedicine is no longer just a trend, it’s a cornerstone of modern healthcare delivery. With growing patient demand for convenience and improved access, investing in telemedicine software development has become essential for healthcare providers, hospitals, and startups alike. From video consultations and remote diagnostics to seamless integration with EHR systems, telehealth software development enables organizations to offer more accessible, efficient, and secure care.
Choosing the right telemedicine software provider plays a critical role in the success of your platform. Whether you’re looking to build from scratch or scale an existing solution, AgileTech, as a trusted telemedicine software development company, offers end-to-end services tailored to your needs. Our team specializes in building user-friendly, compliant, and scalable telehealth software systems that empower both patients and providers.
If you’re ready to transform your healthcare services and stay ahead in the digital health landscape, let AgileTech help you build the best telemedicine software to fit your goals.